In June 2017, I was diagnosed with an autoimmune illness called Lupus, bringing to an end over a decade of unexplained illnesses. It was a relief to get the diagnosis. It helped me put a lot of things into perspective.
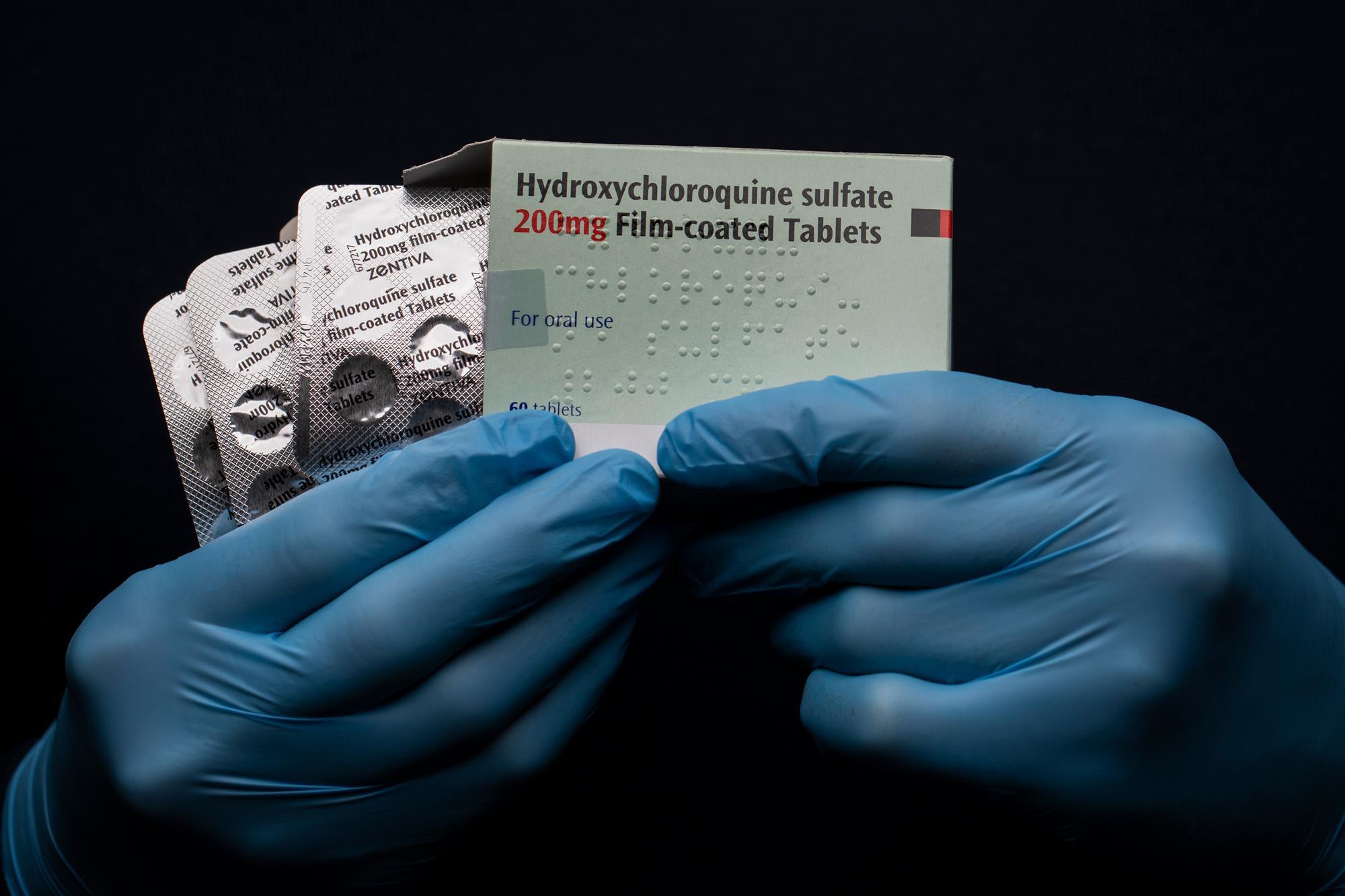
In December of the same year, I met a Ugandan Rheumatologist based in Namibia. He was more familiar with the latest interventions in medicine for Lupus. He recommended that I leave Sulfasalazine which has been prescribed and start using Hydroxychloroquine to treat the Lupus.
Hesitantly, I started its use. In August 2019, I was relieved of all medication. I was in ‘remission’. I had been taking 400mg a day.
My thirst for information and curiosity is what helped me in this journey. I didn’t give up fighting this disease and I knew I would get better. Thus, the right medication led me to remission.
As countries began to lockdown due to the outbreak of the pandemic Covid-19, the end of March, there was a lot of conversation on the drugs that were making patients get better especially in Asia.
Hydroxychloroquine according to some journals was most recommended. Those who lived in Africa in the 1990s should remember this drug. Not so much for its effectiveness but for its side effects. I remember when I started to take it for Lupus, it was recommended that I do an eye exam every 4 months and look out for other changes in my body. Hydroxychloroquine was used for long as an anti-malarial until better drugs got onto the market with fewer side effects. However, it was approved as a DMARD to (disease-modifying antirheumatic drug) to treat Rheumatoid Arthritis and Lupus.
Lupus Support groups, especially on Facebook, began to talk about this as well. Patients from Europe were talking about a shortage.
On March 20th, the first complaint was sounded in a WhatsApp group that has lupus patients from Uganda and Kenya.
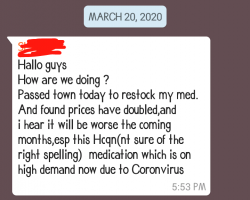
On the same day, the Lupus Foundation of America put out a notice saying that they were aware of the shortage of the drug because it was being used to treat COVID19
“We are actively working with our medical and scientific advisors, other patient groups, partners, and the federal government to take steps that ensure people with lupus will be protected from a disruption in access to critical medications” read the notice.
On 21st March, the President of the US put out a tweet on Hydroxychloroquine and Azithromycin.
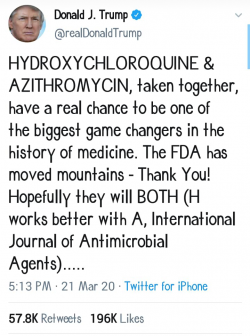
In April, another Lupie in Kenya talked about how hard it was for her to find the medication.
< dir="ltr" lang="en">I got, with a struggle, Hydroxychloroquine (HCQS) for me + 5 other #Lupus patients’ prescriptions. 10 days worth. We need to continue our medication to control Lupus activity. If you have an idea where we can have our HCQS prescriptions filled in Kenya, please reach out…
— 🦋💜 Lupus Awareness Month 🇰🇪 (@Sheblossoms) April 11, 2020
I did not pay attention to the prices in Uganda until this week when one of the Lupus patients asked for help because they only had enough drugs for 3 days before they run out and the pharmacies did not have.
So I texted the two pharmacies I had on my WhatsApp contacts and they both promptly replied. The first didn’t have but recommended the one that I had asked for as well.
The reply read :
We have the UK brand each tablet at 5,000/=
In shock, I did my calculations and realized that if I was still on medication, I would need Ugx 300,000/- a month for my dose. How many people can afford to pay that for a month? As we live through this pandemic, with people losing jobs or their salaries being cut into half – that’s not feasible.
As a Lupie, that was more than my monthly medicine budget then. I had to take 2 more medicines and also had to buy supplements. It just didn’t make sense.
So, I took to Twitter and asked the Ministry of Health, what was going on. To me, while we are handling COVID-19, other patients need access to affordable healthcare. Lupus patients need a lot more care because they are at risk – because of low immunity.
Hydroxychloroquine is going for 5000/– a tablet at @firstpharmacyug
How? B'se #Covid_19?Did the government hoard it all or?
Lupie friends can't get it for treatment. B'se that is 10k per day if on 400mg.Unacceptable! @MinofHealthUG Do something! #LupusAwareness
— Aine (@Ruthaine) May 21, 2020
Lupus patients already have a lot to deal with, the medication allows them to ‘live a little. Uganda’s main national hospital does not have a Rheumatology section. The one rheumatologist that we know who is Ugandan is more academic-focused that most of the patients in the Lupus Support Group have not been helped much by him. When one listens to most of their stories ( we had our first meet up last year) they are sad. Because Uganda’s health system barely recognizes them or even helps them. I am very very privileged that I get to see a Rheumatologist in Nairobi, Kenya. While in remission, I still have to be monitored.
Uganda is using Hydroxychloroquine to treat some of its patients. It had been talked about by the Ministry of Health officials.
The patients we are discharging today were on hydroxychloroquine and erythromycin actually https://t.co/prRo9WdI0o
— Dr. Henry Mwebesa (@henrymwebesa) April 11, 2020
Because Uganda doesn’t have that many cases 175 at the moment – I want to believe that the Ministry of Health can support the patients that need it most.
Lupus and Rheumatoid Arthritis patients in Uganda are feeling the impact of COVID-19 but not like everyone else, it is direr for them.
Will the Ministry of Health respond? I hope so. And I also hope it will not be too late for some of Uganda ‘s most vulnerable citizens.